Health Supervision for
Children With Down Syndrome
The recommendations in this policy statement do not indicate an
exclusive course of treatment for children with genetic disorders, but are meant to
supplement anticipatory guidelines available for treating the healthy child provided in
the AAP publication, "Guidelines for Health Supervision." They are intended to
assist the pediatrician in helping children with genetic conditions to participate fully
in life. Diagnosis and treatment of genetic disorders are changing rapidly. Therefore,
pediatricians are encouraged to view these guidelines in the light of evolving scientific
information. Clinical geneticists may be a valuable resource for the pediatrician seeking
additional information or consultation.
PEDIATRICS (ISSN 0031 4005). Copyright c 2001 by the American Academy of Pediatrics.
ABSTRACT. These guidelines are designed to assist the pediatrician in
caring for the child in whom the diagnosis of Down syndrome has been confirmed by
karyotype. Although the pediatrician's initial contact with the child is usually during
infancy, occasionally the pregnant woman who has been given the prenatal diagnosis of Down
syndrome will be referred for counseling. Therefore, these guidelines offer advice for
this situation as well.
Children with Down syndrome have multiple malformations and mental impairment because
of the presence of extra genetic material from chromosome 21. Although the phenotype is
variable, usually there is enough consistency to enable the experienced clinician to
suspect the diagnosis. Among the more common physical features are hypotonia, small
brachycephalic head, epicanthic folds, flat nasal bridge, upward slanting palpebral
fissures, Brushfield spots, small mouth, small ears, excessive skin at the nape of the
neck, single transverse palmar crease, and short fifth finger with clinodactyly. A wide
space, often with a deep fissure between the first and second toes, is also common. The
degree of mental impairment is variable, ranging from mild (IQ: 50-70) to moderate (IQ:
35-50), and only occasionally to severe (IQ: 20-35). There is an increased risk of
congenital heart defects (50%); leukemia (<l%); hearing loss (75%); otitis media
(50%70%); Hirschsprung disease (<I%); gastrointestinal atresias (12%); eye disease
(60%), including cataracts (15%) and severe refractive errors (50%); acquired hip
dislocation (6%); obstructive sleep apnea (50%75%); and thyroid disease (15%). The social
quotient may be improved with early intervention techniques, although the level of
function is exceedingly variable. Children with Down syndrome often function better in
social situations than might be expected from their IQ.
In approximately 95% of children with Down syndrome, the condition is because of
nonfamilial trisomy 21. In approximately 3% to 4% of persons with the Down syndrome
phenotype, the extra chromosomal material is the result of an unbalanced translocation
between chromosome 21 and another acrocentric chromosome, usually chromosome 14.
Approximately three fourths of these unbalanced translocations are de novo, and
approximately one fourth are the result of familial translocations. If the child has a
translocation, a balanced translocation must be excluded in the parents. If there is a
translocation in either parent, additional familial studies and counseling should be
instituted. In the remaining 1% to 2% of persons with the Down syndrome phenotype, 2 cell
lines are present: I normal and 1 trilsomy 21. This condition is called mosaicism. These
persons, on average, may be phenotypically less severely affected than persons with
trisomy 21 or translocated chromosome 21, but their conditions are generally
indistinguishable in all other aspects.
Medical management, home environment, education, and vocational training can
significantly affect the level of functioning of children and adolescents with Down
syndrome and facilitate their transition to adulthood. The following outline is designed
to help the pediatrician to care for children with Down syndrome and their families. 1-4
It is organized by the issues that need to be addressed in the various age groups (see
Table 1).
Several areas require ongoing assessment throughout childhood and should be reviewed
periodically at developmentally appropriate ages. These include the following:
- Personal support available to family.
- All other financial and medical support programs for which the child and family may be
eligible.
- Supplemental Security Income benefits.
- Injury and abuse prevention with special consideration of developmental skills.
- Diet and exercise to maintain appropriate weight.
THE PRENATAL VISIT
Pediatricians may be asked to counsel a family in which a fetus has a genetic disorder.
In some settings, the pediatrician may be the primary resource for counseling. At other
times, counseling may have been provided for the family by a clinical geneticist,
obstetrician, or developmental pediatrician. In addition, parents may have received
information from a Down syndrome program, a national Down syndrome organization, or an
Internet site. Because of a previous relationship with the family, the pediatrician may be
asked to review this information and assist in the decision-making process. As
appropriate, the pediatrician should discuss the following topics with the family:
- The prenatal laboratory or fetal imaging studies leading to the diagnosis.
- The mechanism for occurrence of the disorder in the fetus and the potential recurrence
rate for the family.
- The prognosis and manifestations, including the wide range of variability seen in
infants and children with Down syndrome.
- When applicable, additional studies that may refine the estimation of the prognosis (eg,
fetal echocardiogram, ultrasound examination for gastrointestinal malformations).
- Currently available treatments and interventions. This discussion needs to include the
efficacy, potential complications and adverse effects, costs, and other burdens associated
with these treatments. Discuss early intervention resources, parent support programs, and
any plausible future treatments.
- The options available to the family for management and rearing of the child using a
nondirective approach. In cases of early prenatal diagnosis, this may include discussion
of pregnancy continuation or termination, rearing the child at home, foster care
placement, and adoption.
If the pregnancy is continued, a plan for delivery and neonatal care must be developed
with the obstetrician and the family. Offer parent-to-parent contact. As the pregnancy
progresses, additional studies may be valuable for modifying this management plan (eg,
detection of a complex heart defect by echocardiography). When appropriate, referral to a
clinical geneticist should be considered for a more extended discussion of clinical
outcomes and variability, recurrence rates, future reproductive options, and evaluation of
the risks for other family members,
HEALTH SUPERVISION FROM BIRTH TO 1 MONTH: NEWBORNS
Examination
Confirm the diagnosis of Down syndrome and review the karyotype with the parents.
Review the phenotype. Discuss the specific findings with both parents whenever possible,
and talk about the following potential clinical manifestations associated with the
syndrome. These may have to be reviewed again at a subsequent meeting.
DISCUSS AND REVIEW
- Hypotonia
- Facial appearance
EVALUATE FOR
- Feeding problems
- Strabismus, cataracts, and nystagmus at birth or by 6 months
- Congenital hearing loss with objective testing, such as brainstern auditory evoked
response or otoacoustic emission at birth or by 3 months 5
- Heart defects (approximately 50% risk). Perform cardiac evaluation (consultation by a
cardiologist
- with expertise and experience in pediatric patients and echocardiogram recommended).
- Duodenal atresia
- Constipation with increased risk of Hirschsprung disease
- Leukemia-more common in children with Down syndrome than in the general population, but
still rare (<l%); leukemoid reactions, on the other hand, are relatively common as is
polycythemia (18%). Obtain complete blood count.
- Congenital hypothyroidism (1% risk)
- Respiratory tract infections
ANTICIPATORY GUIDANCE
- Discuss increased susceptibility to respiratory tract infection
- Discuss the availability and efficacy of early intervention.
- Discuss the early intervention services in the community.
- Inform the family of the availability of support and advice from the parents of other
children with Down syndrome.
- Supply names of Down syndrome support groups and current books and pamphlets (see
"Bibliography and Resources for New Parents").
- Discuss the strengths of the child and positive family experiences.
- Check on individual resources for support, such as family, clergy, and friends.
- Talk about how and what to tell other family members and friends. Review methods of
coping with long-term disabilities.
- Review the recurrence risk in subsequent pregnancies and the availability of prenatal
diagnosis. Discuss unproven therapies. 6-12
HEALTH SUPERVISION FROM 1 MONTH TO I YEAR. INFANCY
- Examination Physical Examination and Laboratory Studies
- Review the risk of serous otitis media (50%-70%). If the tympanic membranes cannot be
visualized, or if the parents express any concern about their child's hearing, refer the
infant to an otolaryngologist. Review the prior hearing evaluation (brainstem auditory
evoked response and otoacoustic emission and refer back to the otolaryngologist and
audiologist if the initial evaluation was abnormal for follow up examination and testing.
A behavioral audiograrn should be obtained at 1 year in all children examined.
- Check for strabismus, cataracts, and nystagmus by 6 months, if not done at birth. Check
the infant's vision at each visit, using developmentally appropriate subjective and
objective criteria. By 6 months, refer the infant to a pediatric ophthalmologist or an
ophthalmologist with special expertise and experience with infants with disabilities.
- Verify results of newborn thyroid function screen. Because of increased risk of acquired
thyroid disease, repeat at 6 and 12 months and then annually. 13,14
- Administer pneumococcal vaccine, as well as other vaccines recommended for all children
unless there are specific contraindications.
ANTICIPATORY GUIDANCE
- Review the infant's growth and development relative to other children with Down syndrome
(Figs 1-4).15
- Review availability of Down syndrome support groups (see "Bibliography and
Resources for New Parents").
- Assess the emotional status of parents and intrafamily relationships. Educate and
support siblings and discuss sibling adjustments. At 6 to 12 months, review the
psychological support and intrafamily relationships, including long-term planning,
financial planning, and guardianship.
- Review the early intervention services relative to the strengths and needs of the infant
and family
- (see "Bibliography and Resources for New Parents").
- Review the family's understanding of the risk of recurrence of Down syndrome and the
availability of prenatal diagnosis.
HEALTH SUPERVISION FROM 1 TO 5 YEARS: EARLY CHILDHOOD
- Obtain a history and perform a physical examination with attention to growth and
developmental status.
- Review the risk of serous otitis media with hearing loss. If the tympanic membranes
cannot be completely visualized (because of the frequent problem of stenotic ear canals),
check the child's audiogram every 6 months up to 3 years or up to when a pure tone
audiograrn is obtained. Refer the child to an otolaryngologist or audiologist if necessary
(approximately 50%-70% risk of serous otitis media between 3 and 5 years).
- Check the child's vision annually, using developmentally appropriate subjective and
objective criteria. Refer the child to a pediatric ophthalmologist or ophthalmologist with
special expertise and experience with children with disabilities every 2 years
(approximately 50% risk of refractive errors between 3 and 5 years).
- At 3 to 5 years, obtain radiographs for evidence of atlantoaxial instability or
subluxation. These may be obtained once during the preschool years. The need for these
studies has been questioned, but they may be required for participation in the Special
Olympics. These studies are more important for children who may participate in contact
sports and are indicated in those who are symptomatic.16-19
- Perform thyroid screening tests annually.
- Discuss symptoms related to obstructive sleep apnea, including snoring, restless sleep,
and sleep position. Refer to a specialist as indicated .20
- Anticipatory Guidance
- Review early intervention, including physical therapy, occupational therapy, and speech,
in the preschool program and discuss future school placement and performance.
- Discuss future pregnancy planning, risk of recurrence of Down syndrome, and prenatal
diagnosis. Assess the child's behavior, and talk about behavioral management, sibling
adjustments, socialization, and recreational skills.
- Encourage families to establish optimal dietary and physical exercise patterns that will
prevent obesity.
HEALTH SUPERVISION FROM 5 TO 13 YEARS: LATE CHILDHOOD
- Obtain a history and perform a physical examination with attention to growth and
developmental status.
- Obtain audiologic evaluation annually. Obtain ophthalmologic evaluation annually.
- Perform thyroid screening tests annually (3%-5% risk of hypothyroidism).
- If appropriate, discuss skin problems: very dry skin and other skin problems are
particularly common in patients with Down syndrome.
- Discuss symptoms related to obstructive sleep apnea, including snoring, restless sleep,
and sleep position. Refer to a specialist as indicated .20
- Anticipatory Guidance
- Review the child's development and appropriateness of school placement and developmental
intervention.
- Discuss socialization, family status, and relationships, including financial
arrangements and guardianship.
- Discuss the development of age-appropriate social skills, self-help skills, and the
development of a sense of responsibility.
- Discuss psychosexual development, physical and sexual development, menstrual hygiene and
management, fertility, and contraception. 21
- Discuss the need for gynecologic care in the pubescent female. Talk about the recurrence
risk of Down syndrome with the patient and her family if she were to become pregnant .22
Review the fact that although there have been 2 case reports in which a male has
reproduced, males with Down syndrome are usually infertile.22
HEALTH SUPERVISION FROM 13 TO 21 YEARS OR OLDER: ADOLESCENCE TO EARLY ADULTHOOD
Examination
- Perform physical examination including CBC and thyroid function tests.
- Obtain annual audiologic evaluation.
- Obtain annual ophthalmologic evaluation.
- Discuss skin care.
- Anticipatory Guidance
- Discuss issues related to transition into adulthood.
- Discuss appropriateness of school placement with emphasis on adequate vocational
training within the school curriculum.20,23 Talk about the recurrence risk of Down
syndrome with the patient and her family if she were to become pregnant.22
- Discuss sexuality and socialization. Discuss the need for and degree of supervision
and/or the need for contraception. Make recommendations for routine gynecologic care.
Discuss group homes and independent living opportunities, workshop settings, and other
community-supported employment. Discuss intrafamily relationships, financial planning, and
guardianship. Facilitate transfer to adult medical care.
fig#1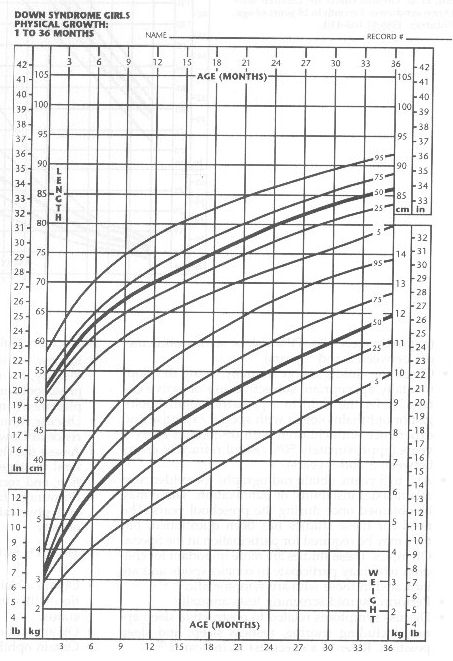
fig#2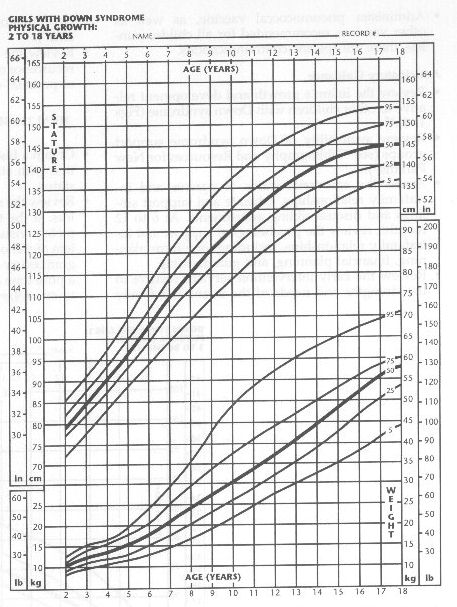
fig#3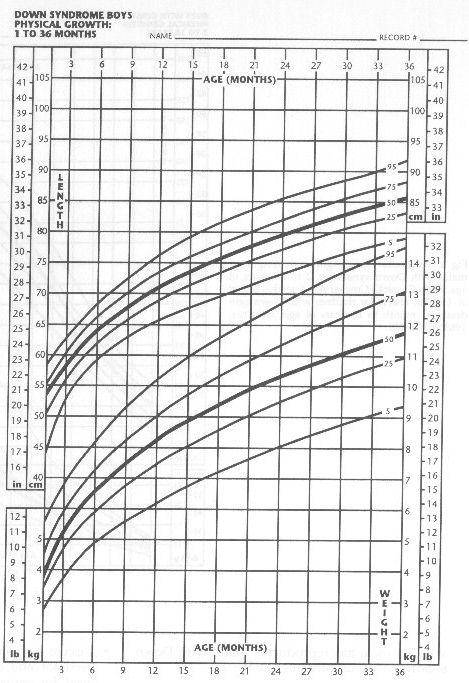
Fig #4 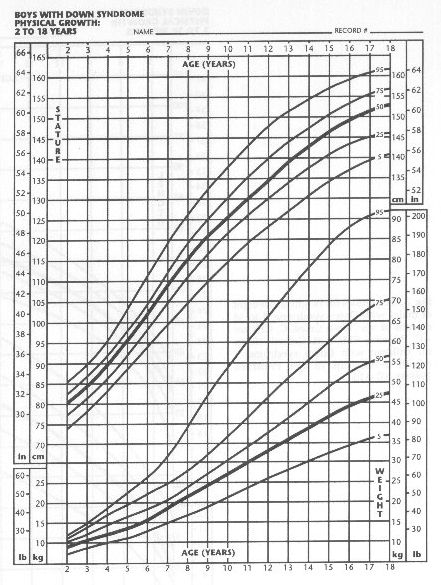
COMMITTEE ON GENETICS, 2000-2001 Christopher Cunniff, MD, Chairperson Jaime L. Frias,
MD Celia Kaye, MD, PhD John B. Moeschler, MD Susan R. Panny, MD Tracy L. Trotter, MD
LIAISONS Felix de la Cruz, MD, MPH National Institutes of Health James W. Hanson, MD
American College of Medical Genetics Michele Lloyd-Puryear, MD, PhD Health Resources and
Services Administration Cynthia A. Moore, MD, PhD Centers for Disease Control and
Prevention John Williams 111, MD American College of Obstetricians and Gynecologists
SECTION LIAISON H. Eugene Hoyme, MD Section on Genetics
CONSULTANTS Marilyn J. Bull, MD William 1. Cohen, MD Franklin Desposito, MD Beth A.
Pletcher, MD Nancy Roizen, MD Rebecca Wappner, MD
STAFF Lauri A. Hall
REFERENCES
- American Academy of Pediatrics Committee on Genetics. Health supervision for children
with Down syndrome. Pediatrics. 1994;93:855-859
- Cohen WI. Health care guidelines for individuals with Down syndrome (Down syndrome
preventive medical checklist). Down Syndrome Q. 1996;1:1-10
- Cooley WC, Graham JM Jr. Down syndrome: an update and review for the primary
pediatrician. Clin Pediatr (Phila). 1991;30:233-253
- de la Cruz F. Medical management of mongolism or Down syndrome. In: Mittler P, de Jong
JM, eds. Biomedical Aspects. Research to Practice in Mental Retardation: Fourth Congress
of the International Associationfor the Scientific Study of Mental Deficiency. Vol 3.
Baltimore, MD: University Park Press; 1977;221-228
- Dahle Al, McCollister FP. Hearing and otologic disorders in children with Down
syndrome. Am j Ment Defic. 1986;90:636 - 642
- National Down Syndrome Congress. Position Statement on Sicca Cell Therapy. Atlanta, GA:
National Down Syndrome Congress; 1989
- Nickel RE. Controversial therapies for young children with developmental disabilities.
Infants Young Child. 1996;8:29-40
- National Down Syndrome Society. Position Statement on Vitamin Related Therapies. New
York, NY: National Down Syndrome Society; 1997. Available at: http://www.ndss.org.
Accessed June 1998
- National Down Syndrome Society. Position Statement on Use of Piracetam. New York, NY:
National Down Syndrome Society; 1996. Available at: http://www.ndss.org. Accessed June
1998
- National Down Syndrome Congress. National intervention in children with Down syndrome.
Atlanta, GA: National Down Syndrome Congress; 1999. Available at:
http://www.ndsccenter.org. Accessed November 1999
- Spigelblatt L, Laine-Ammara G, Pless IB, Guyver A. The use of alternative medicine by
children. Pediatrics. 1994;94(6 pt 1):811-814
- American College of Medical Genetics. Statement on Nutritional Supplements and
Piracetam for Children With Down Syndrome. Bethesda, MD: American College of Medical
Genetics; 1996
- Cutler AT, Benezra-Obeiter R, Brink SJ. Thyroid function in young children with Down
syndrome. Am j Dis Child. 1986;140:479-483
- Karlsson G, Gustafsson J, Heclov G, Ivarsson SA, Anneren G. Thyroid dysfunction in
Down's syndrome: relation to age and thyroid autoimmunity. Arch Dis Child. 1998;79:242-245
- Cronk C, Crocker AC, Pueschel SM, et al. Growth charts for children with Down syndrome:
1 month to 18 years of age. Pediatrics. 1988;81: 102-110
- Davidson RG. Atlantoaxial instability in individuals with Down syndrome: a fresh look
at the evidence. Pediatrics. 1988;81:857-865
- Msall ME, Reese ME, DiGaudio K, Griswold K, Granger CV, Cooke RE. Symptomatic
atlantoaxial instability associated with medical and rehabilitative procedures in children
with Down syndrome. Pediatrics. 1990; 85(3 pt 2):447-449
- Pueschel SM, Findley TW, Furia J, Gallagher PL, Scola FH, Pezzullo JC. Atlantoaxial
instability in Down syndrome: Roentgenographic, neurologic, and somatosensory evoked
potential studies. j Pediatr. 1987;110: 515-521
- Pueschel SM, Scola FH. Atlantoaxial instability in individuals with Down syndrome:
epiderniologic, radiographic, and clinical studies. Pediatrics. 1987;80:555-560
- Pueschel SM, Pueschel JK, eds. Biomedical Concerns in Persons With Down Syndrome.
Baltimore, MD: Brookes Publishing; 1992
- de la Cruz FF, LaVeck GD, eds. Human Sexuality and the Mentally Retarded. New York, NY:
Brunner/Mazel; 1973
- Jagiello G. Reproduction in Down syndrome. In: de la Cruz FF, Gerald PS, eds. Trisomy
21 (Down Syndrome): Research Perspectives. Baltimore, MD: University Park Press;
1981;151-162
- Fenner ME, Hewitt KE, Torpy DM. Down's syndrome: intellectual behavioural functioning
during adulthood. I Ment Defic Res. 1987;31 (pt 3):241-249
BIBLIOGRAPHY AND RESOURCES FOR NEW PARENTS
Bibliography
- Cairo S, Cairo J, Cairo T. Our Brother Has Down's Syndrome: An Introduction for
Children. Toronto, Ontario: Annick Press Ltd; 1985
- Hanson MJ. Teaching the Infant With Down Syndrome: A Guidefor Parents and Professionals.
2nd ed. Austin, TX Pro-Ed; 1987
- Pueschel SM. A parent's guide to Down syndrome. Baltimore, MD: Brookes Publishing; 1990
- Stray-Gunderson K. Babies With Down Syndrome: A New Parents Guide.
- Kensington, MD: Woodbine House; 1986 (English and Spanish editions)
Resources
- March of Dimes, Birth Defects Foundation, 1275 Mamaroneck Ave, White Plains, NY 10605;
Telephone: 914/428-7100
- National Down Syndrome Congress, 1605 Chantilly Dr, Suite 250, Atlanta, GA 30324;
Telephone: 404/633-1555 or 800/232-6372
- National Down Syndrome Society, 666 Broadway, New York, NY 10012; Telephone:
212/460-9330 or 800/221-4602
|